Paid Advertiser
Paid Advertiser
Treatment:
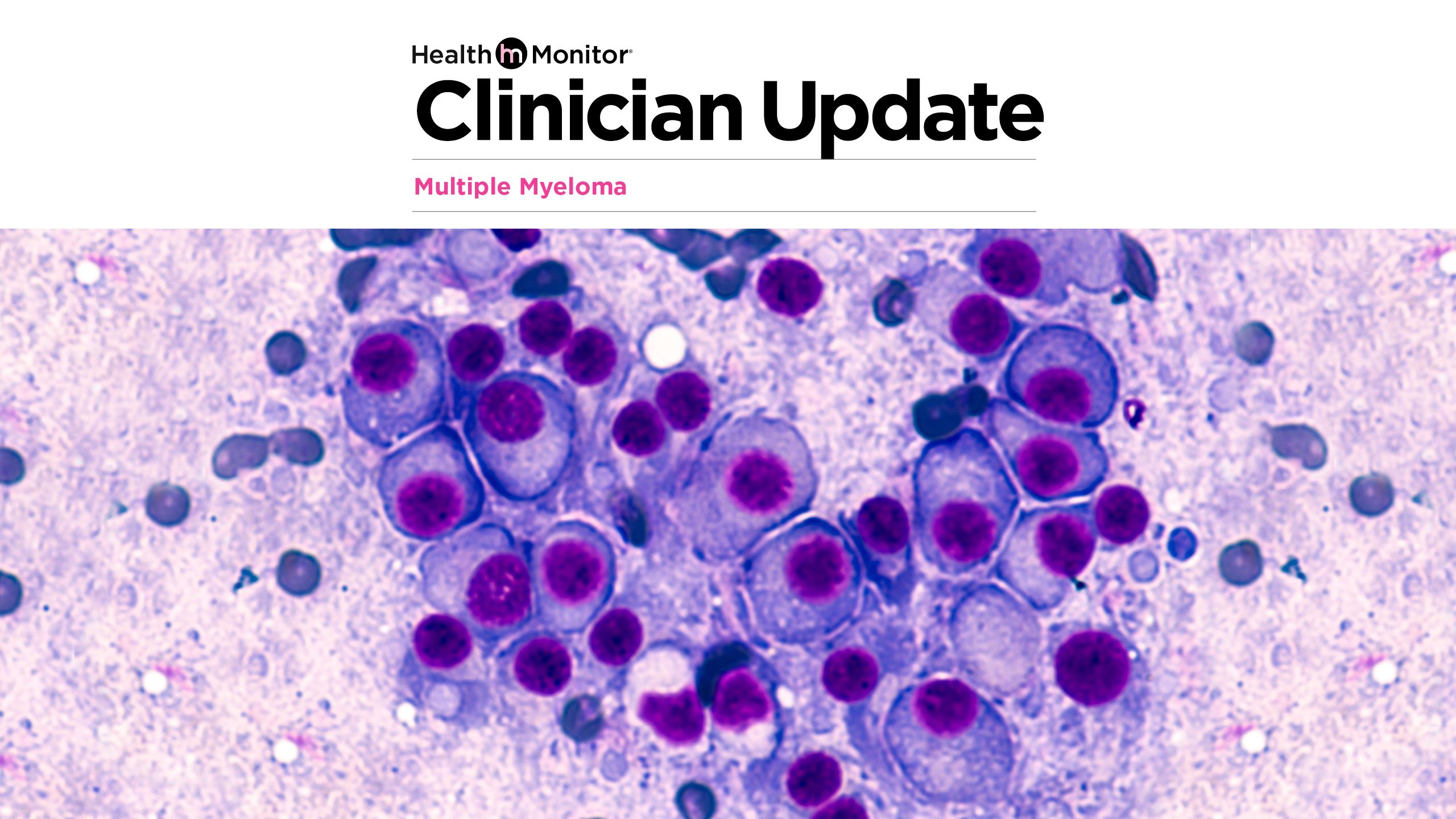
Treating high-risk multiple myeloma after first relapse

Paid Advertiser
Paid Advertiser
Advancements in the treatment of multiple myeloma (MM) have substantially improved outcomes in recent years, with overall response, progression-free survival and overall survival rates continually rising in the wake of a growing armamentarium of therapies.
However, survival benefits have historically been more tempered in patients with high-risk disease.1 Fortunately, improved characterization of high-risk features and an expanding landscape of treatment options within the newly diagnosed and early relapse settings offer an opportunity to similarly improve outcomes for these patients.
Defining high-risk disease
Just as the treatment of MM has advanced, so too has the molecular characterization of disease, which has expanded the definition of high-risk features beyond those used in the revised International Staging System (R-ISS).
“High-risk MM can be defined in several different ways, most commonly by the presence of high-risk cytogenetic features,” explains Muhamed Baljevic, MD, an Associate Professor of Medicine and Director of Plasma Cell Disorders Research and Vanderbilt Amyloidosis Multidisciplinary Programs (VAMP) at Vanderbilt University Medical Center in Nashville.
High-risk cytogenetic features include:2-4
- gain or amplification of chromosome 1 (1q21+)
- del(17p), del(1p)
- t(4;14), t(14;16), t14;20)
- a complex karyotype
Other disease-related factors that are considered high-risk features of relapsed MM include:1-4
- extramedullary disease
- circulating plasma cells (or secondary plasma cell leukemia at relapse)
- early relapse (within 24 months from the start of induction therapy)
Patient-specific factors should be considered as well, Dr. Baljevic emphasizes:
- Refractory to prior therapies. “Prognostic markers that influence outcomes in patients with MM relapse also include patient performance status as well as refractoriness to major anti-MM drug classes (proteasome inhibitors, immunomodulatory drugs, anti-CD38 antibodies) at the time of relapse,” Dr. Baljevic says. “Triple-class or particularly penta-class refractory patients are well described for having poor long-term overall outcomes compared with those patients who are less refractory.”
- Patient-specific characteristics. “General considerations, such as frailty, underlying significant comorbid conditions (e.g., renal impairment) as well as residual toxicities from prior therapies, can all impact how well patients with relapsed or refractory disease can tolerate subsequent therapies,” Dr. Baljevic notes.
Selecting treatment after first relapse
“Optimal treatment of high-risk MM patients in first relapse represents one of the most important areas of unmet need in relapsed/refractory MM,” says Dr. Baljevic.
While it is generally agreed that more intensive therapy is warranted for patients with high-risk disease, appropriate positioning of different therapeutic options—in both the first-line and early relapse settings—remains unclear.3 “Among many different standard of care options, we currently lack randomized control trial data on best choice second-line therapy in relapsed/refractory MM (RRMM), including standard and especially high-risk patients,” Dr. Baljevic explains. “Our understanding of outcomes in these patients comes mainly from subgroup analyses of major trials in RRMM patients who harbor high-risk features.”
When selecting therapy at first relapse, Dr. Baljevic emphasizes that it is important to consider not only disease features and treatment history, but also patients’ wishes and unique needs. “Patient preferences and goals of care, as well as logistics of drug administration (route and frequency of administration) and treatment costs play a significant role in the ultimate decision-making process,” he says. “Patients who are part of underserved communities or demographics can be at a particular disadvantage when it comes to treatment access and subsequent long-term outcomes.”
Anti-CD38 monoclonal antibodies (mAbs) in high-risk patients
“Introduction of anti-CD38 mAbs in the MM armamentarium represents one of the major advances that led to improvement of long-term outcomes for both newly diagnosed MM and RRMM,” says Dr. Baljevic. “Generally speaking, early incorporation of anti-CD38 mAb therapy, particularly for high-risk MM patients, is a preferred choice.”
However, Dr. Baljevic adds, “It is important to note that clinical trials do not have comparative head-to-head data for clear understanding if one drug may be better than the other,” he says. “However, they all conclusively demonstrated the benefit of anti-CD38 mAb containing triplets versus corresponding doublet therapies.”
Illustration by Paul Tong/Ikon Images
Illustration by Paul Tong/Ikon Images
IKEMA subgroup analysis: exceptional PFS
Insights into the effectiveness of anti-CD38 mAbs in high-risk patients have been well-documented in several high-risk subgroups.5-11 The most recent data come from updated IKEMA trial results published in May 2023.12 The study authors reported that subgroup analyses showed consistent progression-free survival (PFS) benefit with isatuximab plus carfilzomib-dexamethasone (Isa-Kd) versus Kd alone across all subgroups, including patients with poor prognoses, such as elderly patients; patients with renal impairment; high-risk cytogenetics including del(17p), t(4;14), t(14;16) or 1q21+ status; and lenalidomide-refractory patients.12 Specifically, data showed a median PFS of 35.7 months after a median 44 months of follow-up, as evaluated by an Independent Response Committee. Further analysis following FDA recommendations on censoring rules showed a median PFS of 41.7 months.
While subgroup analyses from daratumumab specific to patients with the high-risk cytogenetic profile seen in IKEMA are lacking, Dr. Baljevic notes that emerging insights, such as those provided by a recent real-world retrospective study, suggest limited efficacy of daratumumab in this space.13
“Whether this may represent a true difference among daratumumab and isatuximab activity in the 1q21+ space remains to be seen,” he says. “The antitumor activity of isatuximab (in contrast to daratumumab) relies more heavily on antibody-dependent cellular cytotoxicity than complement-dependent cytotoxicity, which may play a role as overexpression of complement regulatory proteins CD55 and CD59 has been implicated in daratumumab resistance in several studies, including patients with 1q21+ changes.”
In addition, Dr. Baljevic notes, “The gene encoding CD55 is localized to 1q32.2 (outside of the 1q21 band), and we may yet learn more how its upregulation could be associated with 1q21+ in relation to sensitivity and/or resistance to different anti-CD38 mAb therapies.”
More convenient modes of anti-CD38 mAb delivery
Subcutaneous (SC) daratumumab has been available to patients for several years, and isatuximab may soon be available in a SC formulation as well. Results from an early-phase trial of SC isatuximab administered via an on-body delivery system demonstrated efficacy and safety profiles consistent with intravenous administration, with no infusion reactions and a high degree of local tolerability.14
“The potential for both drugs to soon be available in SC formulations can only expand the availability and broader incorporation of these agents in all lines of therapy for more optimal long-term MM outcomes,” says Dr. Baljevic.
“Optimal treatment of high-risk MM patients in first relapse represents one of the most important areas of unmet need in relapsed/refractory MM.”
—Muhamed Baljevic, MD
Exploring treatment options
“Early on, it is advisable to try and avoid repeat exposures to therapeutic agents that patients may already be refractory to, considering the variety of available drugs within the same or different classes,” says Dr. Baljevic. “It is essential to establish careful understanding of prior drug exposures versus refractoriness status for all treatment classes, as careful decision-making and choice of subsequent therapies need to be tailored based on these characteristics, particularly with respect to anti-CD38 mAb therapy.”
Dr. Baljevic notes that some physicians (and patients) may prefer to “upgrade” to newer generations of therapies within a given drug class or, increasingly, explore new options with novel mechanisms of action. “The explosion of CAR T-cell and bispecific antibody therapies in RRMM and their continued studying in earlier lines will undoubtedly shape our field for years to come,” he says.
Dr. Baljevic also emphasizes the importance of considering clinical trials for all patients, including those with high-risk disease. “Consideration of clinical trials is always appropriate, especially for high-risk patients, in every phase of disease, from newly diagnosed to highly relapsed/refractory MM,” he notes. “It remains our goal to ensure clinical trials are as representative as possible of different demographic populations, so that data generated can be as broadly applicable as possible. Patients belonging to underserved populations are particularly vulnerable and deserve equal access to care.” (For more on this, see Improving disparities in care for Black patients.)
—by Morgan Meissner
Newly diagnosed high-risk MM:
EMERGING IMPORTANCE OF MRD NEGATIVITY
Minimal residual disease (MRD) is an assessment of malignant cells remaining in a patient’s body following treatment. MRD negative status is defined as the absence of myeloma cells in the bone marrow—and is increasingly being used to assess response in clinical trials, with MRD negativity correlating with better patient outcomes. “Over the years, our ability to test MRD has gradually improved,” says Muhamed Baljevic, MD, Director of Plasma Cell Disorders Research and Vanderbilt Amyloidosis Multidisciplinary Programs at Vanderbilt University Medical Center. “Most recently, mass spectrometry methodologies have further refined our ability to detect minute amounts of disease, and have even been used for screening purposes in high-risk populations.”
In patients with newly diagnosed MM (NDMM), recent clinical trials using quadruplet therapies with anti-CD38 antibodies15,16 have resulted in “fantastic rates of MRD negativity,” Dr. Baljevic says. Now, a new study suggests quadruplet therapy imparts the same benefit for high-risk NDMM—a traditionally difficult-to-treat population. Data from a phase 2 trial (GMMG-CONCEPT) showed that isatuximab + KRd (carfilzomib, lenalidomide and dexamethasone) generated higher MRD-negative remissions in high-risk NDMM, irrespective of transplant status, vs. KRd alone; it also demonstrated a prognostic PFS benefit for MRD negativity.17
The significance: “Patients with high-risk disease generally have a harder time achieving the most optimal and durable responses, which largely translates to shorter long-term overall survivals,” Dr. Baljevic says. "GMMG-CONCEPT is another in a line of fantastic trials that highlight the importance of using the most effective multidrug treatment options in induction, followed by autologous stem cell transplantation for eligible patients, and prolonged consolidation with multidrug maintenance approaches. This can lead to unprecedented rates of sustained MRD negativity, including in patients with high-risk NDMM.”
References
1. Hagen P, et al. High-risk disease in newly diagnosed multiple myeloma: beyond the R-ISS and IMWG definitions. Blood Cancer J. May 30 2022;12(5):83.
2. Costa LJ, et al. Defining and Managing High-Risk Multiple Myeloma: Current Concepts. J Natl Compr Canc Netw. Dec 2020;18(12):1730-1737.
3. Marcon C, et al. Expert consensus on the definition and management of high risk multiple myeloma. Front Oncol. 2022;12:1096852.
4. National Comprehensive Cancer Network. NCCN guidelines: multiple myeloma, version 4.2023. Updated August 25, 2023.
5. Dimopoulos M, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma: results from a randomised, multicentre, open-label, phase 3 study. Lancet. Jul 18 2020;396(10245):186-197.
6. Moreau P, et al. Isatuximab, carfilzomib, and dexamethasone in relapsed multiple myeloma (IKEMA): a multicentre, open-label, randomised phase 3 trial. Lancet. 2021;397(10292):2361-2371.
7. Attal M, et al. Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM): a randomised, multicentre, open-label, phase 3 study. Lancet. Dec 7 2019;394(10214):2096-2107.
8. Dimopoulos MA, et al. Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma: an open-label, randomised, phase 3 trial. Lancet Oncol. Jun 2021;22(6):801-812.
9. Landgren O, et al. Subgroup analysis based on cytogenetic risk in patients with relapsed or refractory multiple myeloma in the CANDOR study. Br J Haematol. Sep 2022;198(6):988-993.
10. Usmani SZ, et al. Final analysis of carfilzomib, dexamethasone, and daratumumab vs carfilzomib and dexamethasone. Blood Adv. Jul 25 2023;7(14):3739-3748.
11. Spicka I, Moreau P, Martin TG, et al. Isatuximab plus carfilzomib and dexamethasone in relapsed multiple myeloma patients with high-risk cytogenetics: IKEMA subgroup analysis. Eur J Haematol. Nov 2022;109(5):504-512.
12. Martin T, et al. Isatuximab, carfilzomib, and dexamethasone in patients with relapsed multiple myeloma: updated results from IKEMA, a randomized Phase 3 study. Blood Cancer J. May 9 2023;13(1):72.
13. Barbieri E, et al. Adverse outcome associated with daratumumab-based treatments in relapsed/refractory multiple myeloma patients with amplification of chromosome arm 1q21: a single-center retrospective experience. Ann Hematol. Dec 2022;101(12):2777-2779.
14. Quach H, et al. P945: subcutaneous isatuximab administration by an on-body delivery system in combination with pomalidomide-dexamethasone in relapsed/refractory multiple myeloma patients: interim phase 1b study results. Hemasphere. Jun 2022;6(suppl):835-836.
15. Costa LJ, et al. Daratumumab, carfilzomib, lenalidomide, and dexamethasone with minimal residual disease response-adapted therapy in newly diagnosed multiple myeloma. J Clin Oncol. 2022;40(25):2901-2912.
16. Goldschmidt H, et al. Addition of isatuximab to lenalidomide, bortezomib, and dexamethasone as induction therapy for newly diagnosed, transplantation-eligible patients with multiple myeloma (GMMG-HD7). Lancet Haematol. 2022;9(11):E810-E821.
17. Leypoldt LB, et al. Isatuximab, carfilzomib, lenalidomide, and dexamethasone for the treatment of high-risk newly diagnosed multiple myeloma. J Clin Oncol. Published online September 27, 2023.
Practice Pearls
Improving
disparities in care for Black patients

Paid Advertiser
Paid Advertiser
Multiple myeloma (MM) is the most common blood cancer in Black individuals, and they have twice the risk of developing MM as White persons.1 In fact, 1 in every 5 patients diagnosed with MM is a Black person, according to an analysis published in the Journal of the National Medical Association.2 The authors found that an estimated 6,910 new cases and 2,360 deaths from MM are expected among Black Americans annually—which accounts for 20% of all new cases and 18% of total deaths from MM each year in the United States.2
“Although huge progress has been made in MM, with average survival improving dramatically in the last 20 years, that benefit has not been seen to the same degree in Black patients,” said Joseph Mikhael, MD, MEd, FRCPC, FACP, Chief Medical Officer of the International Myeloma Foundation (IMF). “This is absolutely unacceptable.”
Delayed diagnosis increases mortality
Not only is MM twice as common among Black Americans compared with White Americans, but their diagnoses are delayed longer as well, says Dr. Mikhael, who is also Professor of Applied Cancer Research and Drug Discovery, Translational Genomics Research Institute at City of Hope Cancer Center. (He notes that diagnosis is often delayed in all patients, but Black persons experience an added delay.) There are many reasons for this, Dr. Mikhael says, including limited access to primary care, limited access to testing, confounding diagnoses like diabetes and limited awareness among the lay public and primary care providers.
Another surprising trend: “The biology of MM in Black patients is generally less aggressive, with a lower risk of the higher-risk forms of the disease,” Dr. Mikhael says. Yet despite this, “mortality in Black patients is twice that of White patients with MM,” he notes.
Lack of access shortens survival
In addition, treatment disparities adversely affect Black populations. “Four advances in myeloma care have improved outcomes in patients, and Black patients have had reduced access to all four,” Dr. Mikhael says. Those advances, which he calls the 4 Ts, are:
- Triplet combinations
- Transplant (autologous stem cell transplants)
- CAR T (chimeric antigen receptor T cell therapy)
- Trials, as in clinical trials
The reasons for this vary, but delayed diagnosis, lack of insurance and lack of culturally sensitive care all play a part. Regarding clinical trials specifically, “Black Americans account for 20% of all MM patients, but only about 5% of those in trials, with even lower percentages in pivotal drug approval trials,” Dr. Mikhael says. He cites systemic racism, lack of trust on the part of Black patients, social determinants of health, implicit bias and the mechanisms of trial design and recruitment among the reasons for these disparities.
Case in point: A SEER study found that the average length of time between MM diagnosis and start of treatment with a novel therapy was 5.2 months for Black patients compared with 2.7 months for White patients. Also, Black Americans were 37% less likely than White Americans to undergo CAR T cell therapy and 21% less likely to be treated with bortezomib; underuse of these treatments is associated with a 12% increased risk of death among Black patients.3
Paradoxically, when Black patients are able to access testing and therapy, “as seen in the VA system,” Dr. Mikhael says, these patients “have improved survival when compared with White patients.” Indeed, a 2022 study found that, while Black patients were less likely to receive novel therapies and CAR T therapy, survival time was comparable between Black and White patients who were treated similarly—and Black patients exhibited significantly longer overall survival than White patients, “reinforcing the importance of equitable access to effective treatment modalities to improve the survival outcomes of Black patients with MM,” the authors concluded.4
Overcoming barriers to quality care
“This is a very complex problem that requires multiple solutions and the coming together of all stakeholders—the public, government, regulators, the healthcare industry and medical professionals,” Dr. Mikhael stresses. To improve care in patients of color, the medical community needs to look at factors beginning as early as diagnosis and continuing through patient education, access to care, affordability and self-advocacy. To help accomplish that, Dr. Mikhael offers the following strategies.
Improve outreach to aid diagnosis. This requires greater MM educational opportunities and awareness of signs and symptoms in the Black community, notes Dr. Mikhael. One key to improved health literacy is through community engagement, which can include distribution of customized materials for Black patients, community-specific events, and leveraging trusted leaders and religious organizations by engaging them to be liaisons with communities of color to create effective health education. To find patient outreach programs, visit the Leukemia & Lymphoma Society (LLS) Myeloma Link initiative at lls.org/myeloma-link.
Educate primary care providers. Improved access to primary care is also critical to facilitate access to testing, early diagnosis and treatment by specialists. Dr. Mikhael cites a study in which he was the lead author that showed that most patients diagnosed with MM initially presented to their PCP, so “generalists must be adept at recognizing typical signs and symptoms with a heightened awareness among particularly high-risk groups such as Black Americans,” he says. The study concluded that MM can be considered in the differential diagnosis with a basic testing strategy that includes a complete blood count, basic chemistry, serum protein electrophoresis, serum free light chain assay, and serum immunofixation electrophoresis, which can then expedite early referral to hematologists/oncologists and prevent delays in both accurate diagnosis and treatment.5 MM specialists can help make a difference by participating in local educational programs for primary care providers, such as those found at Myeloma Link (lls.org/myeloma-link).
Address financial concerns. Insurance issues are often a factor, and improving Black patients’ coverage would go a long way in helping them take advantage of the advances in MM care, says Dr. Mikhael. Start by asking patients if they need help with treatment costs, and make sure they are aware of all their options, including patient assistance and other programs. A list of resources is available from the Multiple Myeloma Research Foundation (MMRF) (themmrf.org/support/financial-assistance-and-transportation) and the IMF (myeloma.org/online-resources/financial-assistance).
Help them access clinical trials. Several institutions—including Vanderbilt University Medical Center, Mayo Clinic Rochester, MD Anderson Cancer Center, University of Colorado Denver, Weill Cornell Medicine and City of Hope National Medical Center—have been awarded Influential Medicine Providing Access to Clinical Trials (IMPACT) research grants, which aim to expand access to high-quality clinical trials for under-represented minority populations with hematologic malignancies. These outreach programs are especially important for patients who live in rural economically disadvantaged areas, as the travel distance to reach academic centers conducting research is often the main barrier to accessing novel therapies (visit lls.org/impact-research-grants).
Ensure culturally sensitive care. The IMF has created the M-Power program “to empower patients and communities to change the course of myeloma—to overcome the disparities,” Dr. Mikhael says (visit mpower.myeloma.org). M-Power encompasses three pillars:
- Engage the community. The program fosters deep community engagement in churches, fraternities and sororities, community centers and other organizations in partnership with multiple groups to raise awareness of the disease, including signs and symptoms, and encourage discussion with their primary care provider.
- Educate the primary care provider. The M-Power program offers an extensive educational platform to facilitate early and accurate diagnosis of MM patients, especially those at higher risk.
- Enhance the care of Black patients. The program hopes to expand the workforce, including “our medical student scholar for health equity program in partnership with the National Medical Association,” Dr. Mikhael says. It also promotes best practices for nurses and physicians, diversity in MM clinical trials and more.
Adds Dr. Mikhael: “Sadly, the disparities are great—in fact, this is the most disparate cancer in the Black community—and has been centuries in the making,” he says. “But the renewed interest in health equity has shined a light on this critical issue. There is a path to reducing the disparity. It will take multi-stakeholder approaches. The IMF M-Power program is an example of how we can address the disparity.”
—by David Levine
To optimize treatment, align with the patient’s goals
A 2023 study in Professional Case Management revealed a surprising discrepancy in perspectives on multiple myeloma (MM) care: What care team members believed were the most important treatment goals for patients were significantly different from what patients reported—including for those of color.6 Specifically, when researchers independently surveyed cancer care teams and MM patients across the United States, they found perspectives differed on the following:
- Biggest challenge: Care team members listed it as the cost of treatment (32% vs. 9% of patients regardless of color), while the majority of patients (32%) listed confidence in their treatment as the biggest challenge.
- Length of survival: 63% of care team members believed this was an important treatment goal, and nearly half of patients agreed—but there were key racial differences. Fewer Black/Hispanic patients cited length of survival as a top goal (38%) vs. 56% of White patients.
- Improvement in quality of life: This was the top goal for 46% of Black/Hispanic patients vs. only 28% of White patients.
The takeaway, according to study authors: Ask each patient about their expectations and treatment goals; explore their concerns and fears; and explain pros and cons of treatment options.
“The biology of MM
in Black patients
is generally less
aggressive…
yet mortality in
Black patients is twice
that of White patients
with MM.”
—Joseph Mikhael, MD
References
1. DeSantis CE, et al. Cancer statistics for African Americans, 2019. CA: A Cancer Journal for Clinicians. 2019 May/June;69(3):211-233.
2. Bhutani M, et al. Disparities in multiple myeloma among African Americans. JNMA. 2023 May;115(2):S26-S31.
3. Ailawadhi S, et al. Racial disparities in treatment patterns and outcomes among patients with multiple myeloma: a SEER-Medicare analysis. Blood Adv. 2019 Oct;3(20):2986-2994.
4. Dong J, et al. Black patients with multiple myeloma have better survival than white patients when treated equally: a matched cohort study. Blood Cancer J. 2022 Feb;12(2):34.
5. Mikhael J, et al. Multiple myeloma for the primary care provider: a practical review to promote earlier diagnosis among diverse populations. Am J Med. 2023 Jan;136(1):33-41.
6. Moreo K, et al. Generating team-based strategies to reduce health inequity in cancer care. Professional Case Management. 2023;28(5):215-223.
Patient Engagement
Helping patients to exercise safely

Paid Advertiser
Paid Advertiser
With the pain, weakened bones and exhaustion that come with multiple myeloma (MM), exercise is often the last thing patients feel like doing. However, as highlighted in a 2023 literature review in the Journal of the Advanced Practitioner in Oncology, physical exercise is not only feasible for MM patients, but it can also help improve their blood counts and bone density as well as fatigue, pain, mood and sleep—in addition to other health benefits such as improved blood pressure and immune function.1
Yet research shows many are hesitant to embark on an exercise program. For example, age-related decline in physical functioning, low self-confidence in physical ability and fear of injury were all cited as major barriers by patients with MM, according to a study in Blood Cancer Journal.2 The authors also noted that the unique features of MM—including increased risk of bone fractures as well as fatigue and weakness—add to the complexity. “Multiple myeloma is different from other cancers when it comes to physical activity,” says study coauthor Elizabeth O’Donnell, MD, Director of Early Detection and Prevention at Dana-Farber Cancer Institute and Assistant Professor of Medicine at Harvard Medical School. “Take, for example, early breast cancer where there’s no bone involvement—you want those patients out and exercising. For patients with MM, you have to make sure they are doing the level of weight-bearing exercise their body can take at that time in their cancer journey,” Dr. O’Donnell says.
In addition, some of the medications used in MM, particularly steroids, can affect muscle mass and cause thinning of the bones. “Not only do you have a disease that has adverse effects, but we give medicines that also can amplify that,” notes Dr. O’Donnell. The good news, she says, is that exercise and physical therapy can help reverse those effects.
However, a recent survey suggests that as many as 50% of cancer care specialists do not offer exercise counseling due to safety concerns, lack of time and lack of knowledge on how to screen for suitability.3 When the patient has MM, counseling becomes even more complicated, notes Dr. O’Donnell. “When someone’s sick with myeloma, there’s so much going. It’s a very medically challenging cancer that affects a lot of different organ systems like the kidneys, blood counts, etc. And if a patient’s not bringing up the topic of exercise, it may be that it’s just not high on their list,” she says.
Such a variety of factors means there is no one-size-fits-all solution, says Dr. O’Donnell. To help personalize an exercise regimen based on each patient’s needs and physical ability, she suggests the following strategies.
Assess their starting point
Dr. O’Donnell says it’s imperative to do a full assessment to establish parameters and necessary modifications. One way to do that is to administer the Physical Activity Readiness Questionnaire (PAR-Q) created by the American Physical Therapy Association (available at apta.org).
What Dr. O’Donnell likes to do: At the end of a patient’s appointment, she walks them out to the front desk. “I like to see how people get out of chairs, get a look at their gait, at how comfortable and confident they are, and with their ability putting on their coat,” she says. This helps her gauge their starting point so she can not only tailor her exercise advice, but also keep an eye on their progress.

Connect them with the right resources
“For people with active disease, you have to be careful—especially with weight-bearing activities,” says Dr. O’Donnell. That’s why she and her study coauthors recommend a multidisciplinary approach combining physical therapy or rehabilitation with standard bone-directed therapy (e.g., zoledronic acid or denosumab) to reduce the risk of bone injury.2
However, it’s important to find out what’s covered by the patient’s insurance, as out-of-pocket costs for a customized plan may be cost-prohibitive. If available, Dr. O’Donnell suggests prescribing physical therapy that focuses on rehabilitation for cancer patients. Another option: Some cancer programs offer physical medicine and rehabilitation (PM&R), which is done with a physical medicine specialist who has completed an additional fellowship in oncology. “To me, this the ideal scenario because you have expertise in oncology and in physical medicine,” says Dr. O’Donnell.
For patients who can’t access or commit to doing physical therapy or PM&R, Dr. O’Donnell recommends the YMCA LIVESTRONG program (visit ymca.org). This recovery program offers supervised group exercise for cancer patients at low or no cost, providing the guidance and camaraderie that may keep them moving. And for home exercisers or those who need a streaming option—as long as they are medically cleared for solo exercise—Dr. O’Donnell offers workouts geared toward cancer patients on the Mass General Cancer Center (MGHCancerCenter) YouTube channel.

“It’s about decreasing sedentary time and trying to stay active. The goal is to encourage patients to preserve their independence.”
—Elizabeth O’Donnell, MD
Redefine “exercise”
For patients with MM, the thought of exercising several days a week can be daunting and even scary due to the risk of fracture. Therefore, Dr. O’Donnell suggests reframing the discussion, especially for those who are frail. “It’s about decreasing sedentary time and trying to stay active,” she says. “The goal is to encourage patients to preserve their independence and daily activities because it correlates with better outcomes,” says Dr. O’Donnell.
To get the conversation started, ask them what they feel confident doing. “People think of exercise as something like running, but there are many other things they can do,” Dr. O’Donnell stresses. She tells patients to focus on increasing time doing activities they enjoy—for example, if they like gardening, encourage them to spend an extra hour working on their plants. When it comes to encouraging movement, Dr. O’Donnell says, “I try to align with people’s lives, what they’re familiar with and what they enjoy.”
Another suggestion from the 2023 review on physical activity in MM: advise patients to get a fitness tracker.1 Dr. O’Donnell likes this approach because, she says, not only does it encourage patients to take more steps throughout the day, but it also helps them gauge their progress.
Discuss pain and fatigue
Fatigue, injuries and pain are also common barriers to exercising with MM.4 Dr. O’Donnell advises addressing these issues directly—and making a patient feel heard and supported—to instill confidence. She also points out that some of the issues holding patients back can actually improve with physical activity. “For example, sleep helps with exercise, and exercise helps us sleep,” she says. The same can be said for pain and fatigue, which may improve as patients get moving.
She advises reassuring patients they can ease into exercise slowly in incremental steps to avoid overexertion. What she says to keep patients motivated: “We want you to live well. The more mobile you are, the more active you are, and the better you’re going to do.”
However, Dr. O’Donnell stresses that it’s not only pain related to MM that could be holding them back—for example, it could also be arthritis. In that case, she says, “Once we get their myeloma well under control, then we start to chip away at the other issues.” And for patients with arthritis who are candidates for joint replacement, “I have had many patients do so and have not had any infectious complications,” says Dr. O’Donnell, adding that they must, of course, be cleared for surgery by their hematologist/oncologist and orthopedic specialist.
—by Beth Shapouri
References
1. Hillengass M, et al. Physical Activity in Multiple Myeloma: A Review of the Current Literature. J Adv Pract Oncol. 2023 Mar;14(2):153-158.
2. Shapiro YN, et al. Lifestyle considerations in multiple myeloma. Blood Cancer J. 2021 Oct 26;11(10):172.
3. Ramsey I, et al. Exercise counseling and referral in cancer care: an international scoping survey of health care practitioners’ knowledge, practices, barriers, and facilitators. Support Cancer Care. 2022 Nov;30(11):9379-9391.
4. Multiple Myeloma: Risk Factors. American Society of Clinical Oncology. Available at cancer.net.
Case Study

Paid Advertiser
Paid Advertiser
PATIENT: SARAH, 45, WAS DIAGNOSED WITH HIGH-RISK 1q21 GAIN IgG Kappa MM IN 2019. HER MEDICAL HISTORY WAS NOTABLE FOR HYPERTENSION, ANXIETY AND DIABETES.
“Long-lasting PFS
in high-risk early
relapse is critical”

Illustration by Juhee Kim
Illustration by Juhee Kim
PHYSICIAN:
Muhamed Baljevic, MD
Associate Professor of Medicine, Director of Plasma Cell Disorders Research and Director of Vanderbilt Amyloidosis Multidisciplinary Programs (VAMP) at Vanderbilt University Medical Center, Nashville
History:
I first saw Sarah when she presented to our facility for a routine checkup, during which slight elevations in her corrected serum calcium and total protein were noted. Serum protein electrophoresis and immunofixation showed 2.8 g/dL of IgG Kappa monoclonal protein. Initial lab findings suggested symptomatic multiple myeloma (MM), which was confirmed on advanced skeletal imaging that showed Sarah had multiple lytic lesions.
Her bone marrow results showed a normocellular marrow with 75% Kappa-restricted plasma cells by CD138 immunohistochemical staining. MM FISH panel showed 1q gain. Gain (3 copies) or amplification (≥ 4 copies) of 1q is a common genetic abnormality that occurs in about 40% of newly diagnosed MM cases. In addition, Sarah was positive for extramedullary disease (EMD) with SUV-avid lymphadenopathy in axillary and inguinal regions as shown on subsequent full body PET-CT examination. Therefore, Sarah was at high risk, with amplification 1q and EMD, each of which has been associated with poorer long-term outcomes.
Sarah, who was married with three adult children, worked as a realtor and had an active lifestyle. She had previously enjoyed outdoor jogging but no longer had the energy, she said, because of fatigue and body aches progressively worsening in the last 6 months.
Sarah and I discussed treatment, including potential adverse effects, and she started therapy immediately. First-line therapy included daratumumab-bortezomib-lenalidomide-dexamethasone quadruplet regimen (initiated as 21-day cycles). Sarah achieved a complete response (CR) to induction therapy and was subsequently consolidated with autologous stem cell transplantation. Following adequate recovery, she was put on additional combination therapy with bortezomib and lenalidomide for a prolonged period, with an eventual aim to transition to single-agent lenalidomide therapy after 2 to 3 years. Sarah additionally underwent dental screening and was started on bone-modifying treatment with denosumab.
Unfortunately, Sarah maintained disease response and control for only 26 months. Her disease relapsed with biochemical progression, manifested in an increase of her M spike to 0.9 g/dL on two consecutive checks during routine follow-up. Additional lab work and bone marrow results indicated evidence of clonal evolution, with the additional 17pdel change on top of 1q21 gain. Due to worsening fatigue and increased bone pain, she received a repeat full body PET-CT scan, which showed new axial skeleton involvement in her lumbar spine as well as emergence of retroperitoneal and periaortic lymph nodes that were suspicious for EMD recurrence as well.
Initiating treatment:
Sarah and I discussed options for second-line therapy. This was a multifactorial decision that had to consider disease features, overall treatment history, her most recent therapy just prior to disease progression, her preference and goals of care, as well as logistics of drug administration (route and frequency).
We discussed choosing a combination treatment in early relapse that would have a good chance to provide a prolonged progression-free survival (PFS) in second-line treatment. To this extent, we determined that Sarah was a good candidate for an isatuximab-containing regimen with carfilzomib. Recent data from the IKEMA trial showed that isatuximab, when used in combination with carfilzomib-dexamethasone, can significantly prolong progression-free survival in high-risk patients and, in particular, those with 1q gain. Again, I counseled her on potential adverse effects before initiating treatment.
Sarah started isatuximab + carfilzomib-dexamethasone (Kd) per the protocol in IKEMA. During cycle 1, her infusion time was decreased to 75 minutes at week 3 due to the absence of infusion-related reactions. At cycle 3 follow-up, Sarah’s labs showed very good partial response and her fatigue and bone pain had resolved.
At cycle 6 follow-up, Sarah showed near CR, with only immunofixation electrophoresis showing evidence of residual IgG lambda M-protein. Bone marrow showed no clonal plasma cells, and Sarah said she felt a lot better. Follow up PET/CT did not reveal any SUV avid lymph nodes. After cycle 12, she was in stringent CR, and she continues to feel well. Sarah and her husband are grateful she has the energy again to enjoy their family and outdoor activities.
Considerations:
High-risk is a broad term that includes MM patients who have certain chromosomal changes, EMD (disease spread beyond the bone marrow compartment) or are refractory to multiple drug classes. All these patients, including those with early relapse (generally considered to be within 24 months from the start of induction therapy), continue to have suboptimal outcomes. In a final analysis of the IKEMA trial after median follow-up of 44 months, treatment with isatuximab + Kd after early MM relapse resulted in doubling of median progression-free survival to approximately 42 months. To date, this is the longest reported PFS from a phase 3 trial regimen in lenalidomide-refractory patients. It is important to remember that to achieve the longest-lasting response after a relapse, it is critical to use the most efficacious treatment early rather than reserving it for later-line therapy. Individualizing therapy for every patient based on their specific needs and disease features is a must. For patients like Sarah with her treatment exposure and disease course, prioritizing regimens with the highest long-term efficacy can improve outcomes and help them live as well as possible for as long as possible.
KOL on Demand
Q&A
Insight on managing relapsing multiple myeloma

Paid Advertiser
Paid Advertiser
Advances in high-risk relapsing MM
Q: What strides have been made in treating relapsing high-risk patients?
A: The landscape of treatment options for relapsed or refractory multiple myeloma (RRMM) is rapidly evolving with the utilization of novel targeted therapies. While treatment of high-risk disease remains a medical challenge, including after first relapse, a series of phase 3 clinical trials that explored multiple triplet combinations showed deeper and more durable responses than had been seen before in patients with relapsed myeloma. In addition, subanalyses of high-risk groups (e.g., high-risk cytogenetic features, refractoriness to major anti-MM drug classes, comorbidities such as renal impairment) confirmed benefits for these patients. This has now resulted in multiple options for therapies combining agents from the three main classes of proteasome inhibitors, immunomodulatory agents and monoclonal antibodies. Quadruplet treatments also are promising in newly diagnosed frontline settings as well as after first relapse. Also, better staging tools will soon be available to assist in identifying early relapses and deep responses to treatment.
Another recent advancement: CAR T-cell treatment has emerged as a promising option for heavily pretreated patients with RRMM and is challenging the paradigm of stem cell transplantation. Similarly, three bispecific antibodies have made it to FDA approval for heavily pretreated patients, and they are on the way for use with earlier lines of therapy. Other targeted treatments receiving more visibility are BCL-2 inhibitors for patients with t(11;14)
mutations.
—Shebli Atrash, MD, Assistant Professor of Clinical Medicine, Wake Forest University School of Medicine; MM specialist at Atrium Health Levine Cancer Institute, Charlotte, NC
Counseling on psychosocial issues
Q: After a patient relapses, what are common psychosocial concerns and how do you address them?
A: This is such a critical question, because at times, as providers we may focus on the physiological and not fully consider the psychological concerns. This becomes an even greater issue as treatments continue advancing and our patients live longer and obtain very deep remissions. There are many psychological concerns that arise in relapsed myeloma, but here are a few highlights of the most common ones.
Fear of relapse may well be the greatest worry—and it is real, especially as we essentially do not cure myeloma at this point. As a result, nearly all patients will relapse, and we often cannot predict the timing of it. Supporting patients throughout their journey is essential, including being a source of hope to them. This is particularly pertinent as we develop more and more therapies.
Another great burden is financial. Often, the disease results in loss of a job, which can be compounded by the high cost of treatment that may be carried by the patient directly. Ensuring we provide financial resources and support is critical, including exploring all options while advocating for policies that reduce the financial burden on patients and their families.
Many of our myeloma patients also experience significant anxiety. This can be related to the disease itself, the treatments given for it and the consequences of both. These cannot be underestimated as the disease is truly life-changing. Interventions should be considered based on a patient’s needs at that time—and should include engagement with the entire myeloma healthcare team and also mental health professionals as appropriate.
Patients can also derive great benefit from meeting with others who have the disease. The International Myeloma Foundation has more than 150 support groups across the United States, which can be searched for by ZIP code at myeloma.org.
—Joseph Mikhael, MD, MEd, FRCPC, FACP, Chief Medical Officer, International Myeloma Foundation; Professor, Applied Cancer Research and Drug Discovery, City of Hope Cancer Center
Offering supportive care
Q: What nondrug therapies can help patients with RRMM?
A: In addition to standard medical treatments, it’s important to discuss nondrug interventions. Complementary and supportive therapies can significantly help manage symptoms and improve the quality of life for individuals with multiple myeloma. To name a few examples:
Physical activity and low-impact exercise are advisable, such as walking, using a stationary bike with low level of resistance or using an elliptical machine, based on their current needs and course of disease. In general, there should be more focus on light exercises. I tell my patients, “The more you do, the better, but if you have muscle soreness the next day it means you overdid it.” (For more, see Helping patients to exercise safely.)
Staying hydrated is important, as myeloma progression is often complicated with dehydration. Adequate hydration can help manage symptoms such as fatigue and constipation and help protect the kidneys from myeloma injury.
Acupuncture appears to be promising and is currently undergoing investigation to explore its capabilities in the treatment of peripheral neuropathy, nausea and fatigue.
Pursuing creative activities can also help patients by reducing stress. These activities—for example, journal writing, taking an art class or doing photography—can offer a sense of accomplishment and distraction from symptoms.
—Shebli Atrash, MD
Paid Advertiser
Paid Advertiser
Clinical Minute:
Special thanks to our medical reviewer:
Muhamed Baljevic, MD, Associate Professor of Medicine, Director of Plasma Cell Disorders Research and Director of Vanderbilt Amyloidosis Multidisciplinary Programs (VAMP) at Vanderbilt University Medical Center, Nashville
Maria Lissandrello, Senior Vice President, Editor-In-Chief; Lori Murray, Associate Vice President, Executive Editor; Lindsay Bosslett, Associate Vice President, Managing Editor; Joana Mangune, Senior Editor; Erica Kerber, Vice President, Creative Director; Jennifer Webber, Associate Vice President, Associate Creative Director; Ashley Pinck, Art Director; Sarah Hartstein, Graphic Designer; Kimberly H. Vivas, Vice President, Production and Project Management; Jennie Macko, Associate Director, Print Production
Dawn Vezirian, Senior Vice President, Financial Planning and Analysis; Tricia Tuozzo, Sales Account Manager; Augie Caruso, Executive Vice President, Sales & Key Accounts; Keith Sedlak, Chief Commercial Officer; Howard Halligan, President, Chief Operating Officer; David M. Paragamian, Chief Executive Officer
Health Monitor Network is the leading clinical and patient education publisher in clinician offices, providing specialty patient guides, clinician updates and digital screens.
Health Monitor Network, 11 Philips Parkway, Montvale, NJ 07645; 201-391-1911; customerservice@healthmonitor.com.
©2024 Data Centrum Communications, Inc.
NAJ24-CU-MM-2RAS
